Definitions :
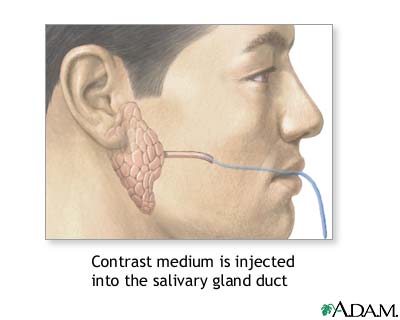
The radiographic demonstration of the major salivary glands by introducing a radiopaque contrast medium into their ductal system.
History :
One of the oldest imaging procedures and was first mentioned by Carpy in 1902.
In 1925, Barsony and Uslenghi described sialography as a diagnostic tool.
Arcelin – 1913 first in vivo sialogram using Bismuth
Equipments
The test is performed in a hospital radiology department or in the health care provider’s office by an X-ray technician. It may also be performed by a dental specialist (an oral and maxillofacial radiologist). You may be given a sedative before the procedure.
You will be asked to lie on your back on the X-ray table. An X-ray is taken before the contrast material is injected to ensure that no stones are present to stop the contrast material from entering the ducts. A catheter (a small flexible tube) will be inserted through your mouth and into the duct of the salivary gland. A contrast medium is then injected into the duct so that the duct will show up on the X-ray. X-rays will be taken from a number of positions.
Preoperative PhaseÂ
Taking scout radiographs for
• To note the position and / or presence of any radiopaque obstruction
• To assess the position of shadows cast by normal anatomic structures that may superimpose the gland
• To assess the exposure factors and patient positioning.
Filling PhaseÂ
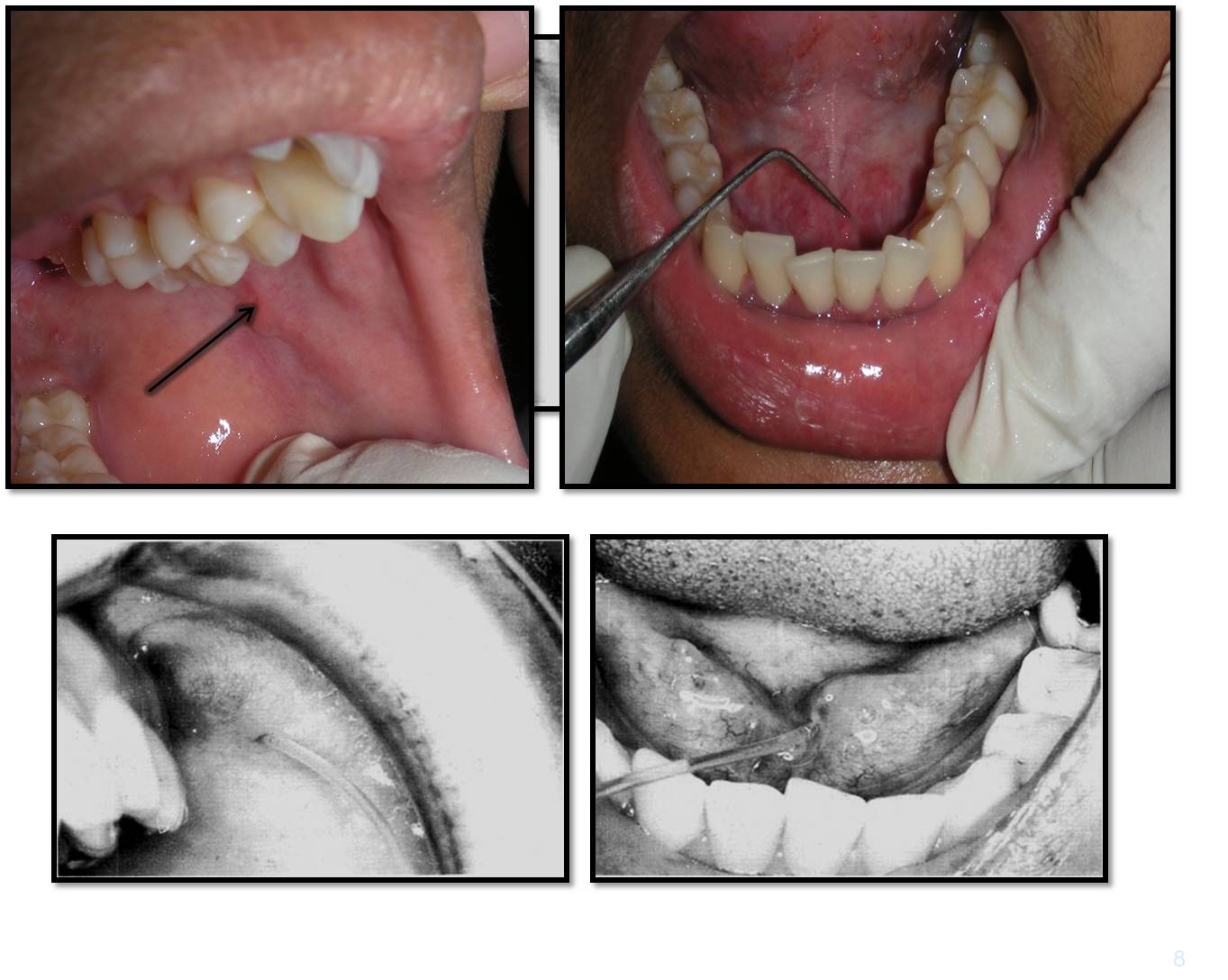
Duct orifice to be located
Probed, dilated and then cannulated using lacrimal probe
The contrast medium introduced.
Radiographs taken , two views at right angles
Emptying PhaseÂ
The cannula removed : patient asked to rinse
Lemon juice / citric acid
I and 5 minutes : Emptying phase radiographs are taken
 Oil Based Contrast Media
ADVANTAGES
Densely radiopaque —- good contrast
High viscosity — slow excretion
DISADVANTAGES
Extravasated contrast media — foreign body reaction
High viscosity – considerable pressure – calculi can be forced deeper
Greater degree of discomfort
Ideal Contrast MediaÂ
Physiology similar to saliva
Miscibility with saliva
Absence of local or systemic toxicity
Pharmacologic inertness
Satisfactory opcification
Low surface tension and viscosity to allow for filling of fine components of the ductal system
Easy elimination and residual solution excreted
IndicationsÂ
Presence and / or position of calculi or other blockages
Extent of ductal and glandular destruction secondary to an obstruction
To determine the extent of glandular breakdown
Assessment of function in cases of dry mouth
To determine the location, size, nature and origin of a swelling or mass
Post operative or post traumatic salivary fistula
Surgical consideration
Amount of damage to gland and its salvageability
Choose site of biopsy
Differentiate intrinsic or extrinsic mass
Relation of mass to facial nerve
Contraindications
Allergy to compounds containing iodine
Periods of acute infection/inflammation
Painful
Retrograde infection
Calculus close to the duct opening : push the calculus back
Anticipated thyroid function tests
Simple Injection TechniqueÂ
Contrast medium introduced using gentle hand pressure
Patient experiences tightness or discomfort in the gland
(about 0.7 ml for the parotid gland, 0.5 ml for the submandibular gland).
ADVANTAGES
• Simple
• Inexpensive.
DISADVANTAGES
arbitrary pressure : Damage to the-gland
– Reliance on patients response : under filling or overfilling of the gland.
Hydrostatic TechniqueÂ
Aqueous contrast media is allowed to flow freely into the gland under the force of gravity until the patient experiences discomfort.
ADVANTAGES
• Less likely to cause damage or give an artifactual picture
• Simple
• Inexpensive.
DISADVANTAGES
• Reliant on the patient’s responses
• Patients have to lie down during the procedure, so they need to be positioned-in advance for the filling-phase radiographs.
Continuous Infusion Pressure Monitored TechniqueÂ
A constant flow rate is maintained and the ductal pressure monitored throughout the procedure.
ADVANTAGES
• The controlled introduction of contrast media at known pressures -no damage
• Does not cause overfilling of the gland
• Does not rely on the patient’s responses.
DISADVANTAGES
• Complex equipment is required
• Time consuming.
 Normal Sialographic Appearance of the Parotid Gland
The main duct is of even diameter (1-2 mm wide) filled completely.
The duct structure within the gland branches -regularly and tapers gradually towards the periphery of the gland, the so-called tree in winter appearance
 Sialographic Appearance of Submandibular Gland
The main duct is of even diameter (1-2 mm wide) filled completely.
The duct structure within the gland branches -regularly and tapers gradually towards the periphery of the gland, the so-called tree in winter appearance
Sialographic appearances of sialadenitis
Dots or blobs of contrast medium within the gland , an appearance known as sialectasis caused by the inflammation of the glandular tissue producing saccular dilatation of the acini.
– The main duct is usually normal.
APPLE TREE IN BLOSSOM
Sialographic appearance in Sjogren’s Syndrome
Widespread dots or blobs of contrast medium within the gland, an appearance known as ‘punctate sialectasis’ or ‘snowstorm’ or ‘branchless fruit laden tree’, or ‘cherry blossom’ appearance.
– Retention of the contrast medium during the emptying phase.
– Main duct normal.
Interventional Sialography
minimally invasive interventional procedures
balloon catheters and small Dormia baskets under fluoroscopic guidance.
Sialographic Appearance of Intrinsic Tumour
– An area of under-filling within the gland, due to ductal compression by the tumor.
– Ductal displacement – “ball in handâ€.