Continued from Part 2
Chronic infections
Chronic candidal infection
This is often associated with speckled leukoplakias and such lesions are particularly prone to undergo cancerous transformation, though the role of candidal or yeast infection in malignant transformation must be regarded as uncertain.
Syphilis
Historically tertiary syphilis has been linked with cancer of mouth. However late-stage syphilis is now exceedingly rare and its relevance to the cause of oral cancer today is insignificant.
Premalignant lesions and condition
A precancerous (or a premalignant) lesion is defined as a morphologically altered lesion in which cancer is more likely to occur than in its apparently normal counterpart, for example leukoplakia, erythroplakia, and erythroleukoplakia. That is, the lesion itself undergoes cancerous transformation. In contrast, a precancerous (or premalignant) condition is a generalized state associated with a significantly increased risk for cancer, for example oral submucous fibrosis.
The following may be described as precancerous lesions or conditions of the oral mucosa:
Precancerous lesions
- Leukoplakia – homogenous, non-homogenous, nodular and speckled types, including candida-associated lesions (chronis hyperplastic candidosis) and profilerative verrucous leukoplakia
- Erythroplakia
- Carcinoma in situ
Precancerous conditions
- Oral submucous fibrosis
- Lichen planus
- Actinic keratosis (for cancer of the lip)
- Other conditions associated with epithelial atrophy, for example sideropenic dysphagia.
How do oral cancers develop?
Cancers result from changes (mutations) in genes which control cell behaviors. Mutated genes may result in a cell which grows and multiples at an uncontrolled rate, is unable to repair DNA damage within itself, or refuses to self destruct.
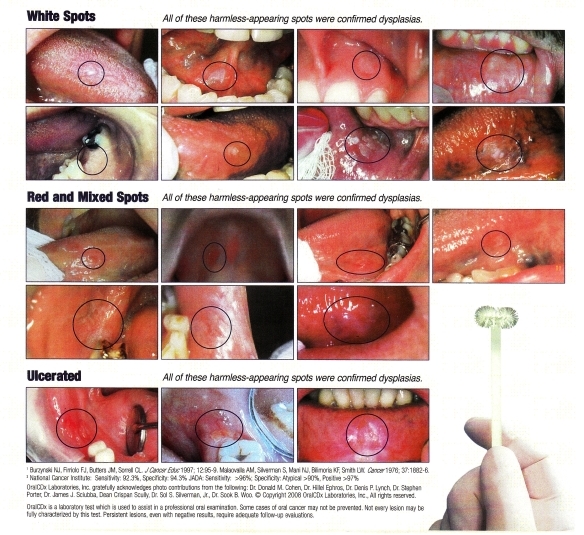
How does oral cancer appear clinically?
Oral cancer symptoms are most often seen as:
- A persistent painless ulcer that bleeds easily and does not heal
- A lump, thickening, rough spot, crust or small eroded area
- Color changes such as an area of white patch (leukoplakia), a red-white patch (erythroleukoplakia) or a red patch (eryhtroplakia),
- Difficulty in chewing, swallowing, speaking or moving the jaw or tongue
- Changes in the voice
- A change in the way your teeth fit together
- Pain, tenderness or numbness in the mouth or lips
- Signs of hardness or fixation of lesion
- Regional extension to draining lymph nodes
- As cancerous change of long-standing harmless (benign) tumors or rarely, cyst linings or a non-healing extraction socket.
Malignancy should be suspected if any of the above lesions persists for more than three weeks. The ulcer is described as a form with raised edges, with an indurated, inflamed, granular base and is fixed to surrounding tissues.
Pain is usually a late feature when the lesion becomes superinfected or during eating of spicy foods. Referred ear pain (otalgia) is a common manifestation of pain from oral and particularly tongue or oropharyngeal cancer.
How is oral cancer screening done?
Extraoral examination
The examination includes inspection of the head and neck. Any asymmetry of changes on the skin such as fissuring, growths and/or color change is noted down. The regional lymph node areas are palpated on both sides to detect any enlarged nodes.
The perioral and intraoral examination procedure follows a seven-step systematic assessment of the lips, labial mucosa and commissures, buccal mucosa and commissures, gums and alveolar ridge, tongue, floor of mouth and hard and soft palate.
Perioral soft tissue examination
Lips
The lips are observed both closed and open. The color, texture and any surface abnormalities of the upper and lower vermillion borders is noted
Intraoral soft tissue examination
Labial mucosa (the soft tissues facing the lips)
With the mouth partially open, the labial mucosa and sulcus of the upper vestibule and frenum, and the lower vestibule is visually examined. The color, texture, swelling or other abnormalities of the vestibular mucosa and gums is observed.
Buccal mucosa (cheeks)
The right and left buccal mucosa extending from the labial commissures and back to the anterior tonsillar pillar is examined. Any change in pigmentation, color, texture, mobility and other abnormalities of the mucosa is noted
Gums
The buccal (cheek), palatal (palate), lingual (tongue) and labial (lips) aspects of the gums and alveolar ridges (processes) are examined.
 Tongue
With the tongue at rest and mouth partially open, the upper surface of the tongue is inspected for any swelling, ulceration, variation in size, color or texture. Any change in the papillae covering the surface of the tongue is noted and the tip of the tongue is examined. The tongue is the protruded and any abnormality of mobility or positioning is noted.
The tip of the tongue is grasped with a piece of gauze to assist full protrusion and will aid examination of the more posterior aspects of the tongue’s lateral borders. With the aid of mouth mirrors, the left and right side margins of the tongue are inspected.
The lower surface of the tongue is palpated to detect any growths or abnormalities.
Floor of mouth
With the tongue still elevated, the floor of the mouth is inspected for changes in color, texture, swellings or other surface abnormalities.
Hard palate
With the mouth wide open and the patient’s head tilted back, the base of the tongue is depressed with a mouth mirror, inspecting the hard palate
Oropharynx (the part of the throat at the back of the mouth)
The soft palate and oropharnygeal tissues are examined.
To be continued in Part 4