The female body undergoes many changes during pregnancy that include changes within the mouth. Hormonal imbalances affect the mouth by changing the bacteria already present in the mouth and altering the types of bacteria that grow in plaque. Below are the few conditions you may encounter during your pregnancy period:
Pregnancy-induced gingivitis

Pregnancy gingivitis
A type of sex steroid hormone gum disease most commonly seen in the second trimester of pregnancy, pregnancy-induced gingivitis (gums inflammation) is characterized by an exaggerated response to plaque biofilm in the mouth.
The gums may appear fiery red at the margins and the gums between the teeth appear swollen and enlarged with absence of bone and attachment. The gum tissues may be swollen, smooth and shiny; bleed easily and have deep gum pockets. These gum changes occur earlier and more frequently in the front of the mouth than in the behind areas and may progress to a pregnancy granuloma.
Gingivitis during pregnancy usually reaches maximum severity during the eighth month and is less severe after childbirth. However the tissue does not necessarily return to a state of health. A strict oral hygiene regimen is required to restore gums to original state.
As the most frequent oral appearance in pregnancy, pregnancy-associated gingivitis is due to poor oral hygiene, local irritants and a shift in the predominant types of bacteria in the mouth. Gingivitis is made worse by hormonal and blood vessels changes and the presence of increased anaerobic bacteria that proliferates in the high progesterone environment during pregnancy. The sex steroid hormones (estrogen and progesterone) increase gingivitis in pregnancy as they serve as nutrient for bacteria to grow.
Pregnancy granuloma (pyogenic granuloma)
Pregnancy granulomas or pregnancy tumors are single, tumor-like, soft tissue growths typically seen on the gums region between teeth and they rarely destroy the bone. They are attached via a stem with intense red to deep purple color, depending on the blood supply of the lesion and the degree of blood stagnation.
Usually no larger than 2 cm, the granulomas are painless and may bleed readily if disturbed. They usually regress after delivery and are often related to poor oral hygiene. Furthermore pregnancy graunulomas are attributed to the general effects of progesterone and estrogen on the host immune system.
Management for granuloma of pregnancy is to wait until after delivery for surgical removal. However situations may dictate immediate removal when the granuloma is painful, when it disturbs the position of teeth or when it bleeds easily. If surgical removal is necessary, it is best to remove it during the second trimester because of the low risk to the fetus during this time period. If removed during pregnancy, the granuloma may recur therefore an additional surgical procedure may be needed after delivery.
Tooth mobility (loose teeth)
Loose teeth are sometimes present and may be related to disturbances in the attachment of the teeth. Movement of teeth usually reverses or declines after delivery.
Perimylolysis (erosion of teeth)
Acid erosion of the teeth is rare in pregnancy but may occur if a pregnant woman vomits repeatedly, as may be the case with severe morning sickness. Erosion of the surfaces of the teeth occurs when the crowns of the teeth is stripped of its minerals and softened by gastric acids. Further mechanical erosion in pregnancy could then occur when the tongue or toothbrush moves against the teeth.
Management of acid erosion of teeth is to rinse with water immediately after vomiting and before brushing your teeth. You can make your own mouth wash using baking soda to neutralize the acid in the mouth. Your dentist may recommend you to use at-home fluoride rinses or gels to protect your teeth.
Oral Thrush
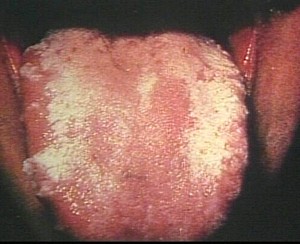
Mouth infection by Candida albicans, a type of yeast, can lead to candidiasis or more commonly known as thrush. Candida normally lives harmlessly in the mouth but under certain conditions like pregnancy, it may multiply out of control due to disturbance of the hormonal balance in the body.
Thrush is superficial and appears as a thick white coating on the affected tissues for example the tongue, cheeks and gum tissues; resembling milk curds. The coating can be wiped away, leaving a red, raw and often bleeding base. The yeast infection can occur anywhere in the mouth and vary in size from small, drop-like areas to plaques covering a wide area.
Oral thrush can be diagnosed by your dentist by analyzing the white curds scrapped off from the mouth and anti-fungals are usually prescribed to manage the condition.
How to manage the changes in your mouth
- Eat fresh fruits regularly like pineapple which has enzymes that clean the mouth.
- Practice good oral hygiene with proper tooth brushing techniques and the usage of floss and mouthwash
- Make regular appointments with your dentist to ensure your mouth stays in a healthy condition
- Maintain good general health by having proper nutrition and exercise
When to see a doctor or dentist
You should visit your attending doctor or dentist when any of the above conditions is causing you pain and discomfort or show signs of infections.



Pingback: Causes of Gum Swellings and Lumps Part2 | Intelligent Dental
Brush your teeth and gums routinely. For most people that means brushing at least two times per day, or at the minimum after each meal. When you do brush you should make a point to do so for at least five minutes.Floss routinely. Flossing is important for preventing gingivitis and periodontal disease. Try a thin floss or waxed floss if you find your gums are sensitive during pregnancy.
You can not believe how long ive been looking for something like this. Browsed through 10 pages of Yahoo results without finding anything. Quick search on Bing. There was this… Really have to start using it more often!
Pingback: How Diabetes Can Affect Your Oral Health Part 1 | Intelligent Dental
Pingback: What is Oral Pyogenic Granuloma? | Intelligent Dental