INDICATIONS OF LOCAL ANESTHESIA
1. Extraction and odontectomy
2. Alveoloplasty and alveolotomy
3. Incision and drainage of abscess
4. Cavity preparation in deeper cavities
5. Pulp procedure
6. Periodontal and gingival surgery
7. Cyst enucleation and marsupialization
8. Removal of small benign growth and salivary stones
9. Relief from denture sore spots
10. Treatment of trismus
11. Diagnostic test for various facial pain esp. trigeminal neuralgia
12. As a treatment therapy for trigeminal neuralgia
13. In radiography when patient is gagging.
14. For anesthesia of oral cavity and jawbones in treatment of fractures
CONTRAINDICATIONS OF LOCAL ANESTHESIA
1. Fearful and apprehensive patients
2. Allergy to LA solution
3. Acute infections, fear of needle contamination and spread of infection
4. Mentally retarded, uncooperative or very young children
5. When anatomic anomalies make anesthesia difficult or impossible
6. Hyperthyroidism
7. Liver disorders
8. Renal disorders
9. Cardiac patients
10. Uncontrolled diabetic patients
11. Patients with any internal hemorrhage
12. Major oral surgical procedure
ADVANTAGES OF LOCAL ANESTHESIA
1. Patient is awake and cooperative
2. Patient does not have to omit the previous night meals as in GA
3. No trained person required
4. Negligible incidence of morbidity
5. Patient can leave the dental clinic unescorted
ARMAMENTARIUM
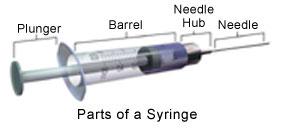
SYRINGES
Types:
1) Non Disposable:
– Breech – loading, metallic, cartridge type, Aspirating.
– Breech – loading, Plastic, cartridge type, Aspirating.
– Breech – loading, metallic, cartridge type, Self Aspirating.
– Pressure Syringe.
– Jet Injector.
2) Disposable Syringes
3) Safety Syringes
4) Computer Controlled Local Anesthetic Device (CCLAD)
NEEDLES
Permits the anesthetic solution to travel from the syringe into the tissues surrounding the needle tip.
PARTS :
 Bevel (Long, Medium & Short)
 Shaft
 Hub
 Syringe Adapter
INFILTRATION (FIELD BLOCK) ANESTHESIA
The principle of infiltration analgesia is the injection of anesthetic solution very near the actual area to be treated and relying upon the solution diffusing or infiltrating to the sensory nerves so that conduction pain impulses prevented.
Main types
 Submucous and Supraperiosteal
Subperiosteal
Intraligamentary
Intraoosseous
Papillary
 Â
PERIODONTAL CONSIDERATIONS
Control of intra-op hemorrhage
Soft tissue manipulation is associated with hemorrhage esp. when tissues are not healthy.
LA with vasodilating properties proves to be counterproductive
Hence addition of vasoconstrictors is beneficial
Epinephrine is the drug of choice.
Excessive use may cause rebound bleeding
Â
Long duration procedures
During longer duration procedures (2 hours or more) bupivacaine a long acting LA is preferred.
However, according to Danielsson bupivacaine has long duration of action when used for regional nerve block (Int. J. Oral Maxillofac Surgery 15,119 -126,1986)
But its duration of action when used as supraperiosteal injection is somewhat shorter even than that of lidocaine with epinephrine
Post op analgesic period of bupivacaine is 8 hrs in mandible and 5 hrs in maxilla
Post-procedural pain control
Long acting LA’s offer a means to achieve post op pain control with minimal risk of developing adverse reactions unlike opiod analgesics
                 Often intermediate LA used intra-op and long acting LA at the end of the procedure
However this is contraindicated in children and physically and mentally incapacitated patientsÂ
Â
NEWER ADVANCES
Centbucridine – most of the research in relation to this drug has been conducted in India by Gupta et al, Suri et al.
 It is a quinolone derivative, 5 – 8 times more potent than Lidocaine.
Does not affect the CVS and CNS adversely
Only trial in dentistry showed it to be as effective in 0.5% concentration, as Lidocaine 2% (Vachrajani et al)
Â
 Ropivacaine – Long acting amide. It is prepared as an isomer while all other amide linked anesthetics are available as racemic mixture
It has a greater margin of safety between convulsive and lethal doses, it is less dysrhythmogenic, has a shorter half life and decreased cardiotoxicity than bupivacaine.
Â
EMLA – 5% Lidocaine and 5% prilocaine (25mg/kg) in a oil in water emulsion
It could to some extent eliminate the use of needle esp. for minor procedures.
Â
pH alterations– by Addition of sodium bicarbonate
Addition of CO2
CO2Â Â diffuses through the nerve membrane and decreases the intracellular pH and increases the intracellular concentration of RNH+
Thus the anesthtetic becomes concentarated within the nerve trunk (ion trapping). This increases the duration of anesthesia
However the drug must be administered shortly after mixing with CO2
Â
Hyaluronidase– addition of this increases both the onset and area of anesthesia.
Duration of anesthesia is slightly decreased
It should be added to anesthetic cartridge just before administration
Â
Ultra long-acting LA- Tetrodotoxin and Saxitoxin are highly toxic, hence their use is not advocated
Â
Slow release of LA for patients with chronic pain, where prolonged analgesia has been desired
2 diff approaches have been tried:
Insertion of bupivacaine into egg phospholipid and cholesterol liposomes
Incorporation into polylactic acid microspheres
Â
Other methods of inducing local anesthesia
Electronic dental anesthesia (EDA)
Mechanism of action of EDA can be explained by the gate control theory. Vibrating, pulsating, twitching stimulates the large A fibres, which activates the inhibitory interneuron and closes the gate. Pain impulses produced by scalpel or high speed drill are transmitted via the smaller fibres which come on the closed gate and their conduction is blocked
Also the blood levels of serotonin, endorphins and enkephalins are increased, these act like systemic analgesics decreasing the pain perception of the patient
EDA has been used with great success in nonsurgical periodontics.
EDA can be used for obtaining pain control during LA administration. This   produces excellent soft tissue anesthesia…study by Meechan et al.
The elevated levels of serotonin and β-endorphin levels after EDA reduces pain in post op period.
It can be used for reversing local anesthesia in patients with risk of post-op anesthetic complications.
Contraindications of EDA:
Cardiac pacemakers
Neurological disorders
Pregnancy
Very young pediatric patient
Older patients with senile dementia
Language communication difficulties
Â
Â
Â
Â
IN MEDICALLY COMPROMISED PATIENTS
Bleeding disorders – aspiration is a must, avoid nerve blocks, infiltration and intraligamentary injections preferred.
Congestive heart failure – Decreased liver perfusion leading to increase in half life, therefore increased chance of toxicity
Myocardial infarction – treatment avoided for 6 months, limited use of vasoconstrictor (0.04 mg).
Thyroid disease – avoid epinephrine
Hypertensive patients – BP to be checked before every appointment.
Renal diseases – decreased clearance, therefore, high level of anesthetics in blood hence, increased chance of toxicity
Atypical plasma cholinesterase – avoid ester linked LA
Malignant hyperthermia – was thought to be precipitated by amide linked Las however there is no concrete proof to the same
Methhemoglobinemia – caused due to the major metabolite of prilocaine i.e. orthotoluidone. Hence used cautiously in susceptible patients.
Â
Drug interactions
Cimetidine –Â It competes with lidocaine for binding with hepatic oxidative enzymes
Suphonamides – ester linked LA thought to decrease their bacteriostatic action
Opioid analgesics– may increase the risk of LA overdose
Tricyclic antidepressants – Enhances the CVS actions of exogenously administered vasopressors leading to hypertensive crisis
Nonselective betablockers– cause  increase in BP and reflex bradycardia if given along with vasopressors
General anesthetic – esp. halogenated general anesthetics increase risk of cardiac dysrhythmias
Cocaine – it itself causes massive vasoconstriction and deprives the heart of oxygen. Hence Local anesthetic agents without a vasopressor preferred in these cases
For complications of LA, refer to : Â http://www.intelligentdental.com/2011/10/22/complications-of-injections-part-1/