Continued from Part 1
Drug reactions
- Epanutin/phenytoin/dilantin/DPH – an anticonvulsant drug given to epileptics, some degree of gums enlargement occurs in a large percentage of epileptics taking phenytoin, especially in those under 40 years of age.
- Cyclosporine – an immunosuppressive drug, it can produce fibrous hyperplasia of the gums. The condition is however less common in patients on cyclosporine, but when it occurs it may be very severe.
- Nifedipine – a calcium channel blocking drug given to treat cardiac angina, arrhythmias and hypertension, it produces fibrous hyperplasia of the gums. Nifedipine hyperplasia is less firm than the other two, and contains a higher proportion of ground substance.
Clinical features of drug-induced gums enlargement
The gums on the outer surface of the front teeth are more severely affected than back teeth. The swelling is fibrous – firm, pink and lobulated, and the swelling does not appear to be severe if oral hygiene is good. With superimposed inflammation the gums, swelling can become soft and red and bleed when provoked. The gum enlargement can almost cover the teeth though the size of the swelling not related directly to drug dosage.
Mechanism of drug-induced gums enlargement
- Influence fibroblast function by folic acid depletion and decreasing its permeability to calcium therefore increasing collagen in gums.
- Effects in androgen metabolism by involving testosterone which affects fibroblast
- The drug selects a subpopulation of fibroblasts that produce large amounts of collagen
- The drug also decreases the amount of phagocytosed collagen with fibroblasts
Management of drug-induced gums enlargement
Changing the drug rarely possible therefore treatment is restricted to oral hygiene instructions and scaling of gumline. Local removal of overgrowth tissue can be done by gingivectomy however recurrence is common 3 to 6 months later.
Hereditary conditions
Down’s syndrome (chromosome 21 trisomy)
Caused by commonly non-dysjunction during oogenesis and rarely reciprocal translocation of groups 13-15 and 21-22, incidence of Down syndrome is 1:700 births increasing to 1:100 with mothers over 45.
There is varying degree of metal handicap with mongoloid facial features, and individuals are prone to infections and 20 times incidence of leukemia.
Oral aspects of Down’s syndromes
Typically class III occlusion with anterior open bite seen and there is a large tongue and a lack of lip seal. Furthermore there is an increased incidence of chronic periodontitis and increased susceptibility to acute necrotizing ulcerative gingivitis (ANUG).
Oral care of Down syndrome people
Frequent monitoring and prompt treatment of any problem should be done. Good plaque control and frequent scaling are important and the caretakers may have to finish off the plaque control.
Hereditary gingival fibromatosis
This autosomal dominant trait with an incidence of 1:350,000 can occur singly or in association with other inherited syndromes though there is also a fairly common idiopathic version.
Hereditary gingival fibromatosis is revealed on eruption of teeth, usually permanent teeth, with excessive production of collagen in the gums corium. The condition can be generalized or localized, delaying tooth eruption and the cause seems to be permanently activated fibroblasts.
Granulomatous conditions
Crohn’s disease
Crohn’s disease is a chronic inflammatory condition affecting any part of the gut from the mouth to the anus with regional enteritis primarily of the terminal ileum. There is stenosis (abnormal narrowing of a bodily canal or passageway) with necrotic breakdown and scarring of gastrointestinal tract and other gastrointestinal areas are also affected including the mouth.
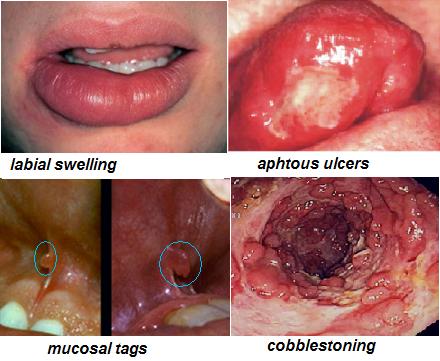
Oral manifestations of Crohn’s disease
- A cobblestone appearance of the oral cheek mucosa
- Labial and buccal gum swellings with mucosal tag
- Fissuring of the midline of the lip
- Aphthous-like ulceration and angular cheilitis
- Enlargement of the attached gums which are diffuse, red and granular
- Severe periodontal disease is seen in these individuals but there is usually a good response to normal periodontal therapy
Hematological conditions (blood disorders)
Relevance of blood disease in chronic periodontal disease
Blood disorders are not causes of chronic periodontal disease but can be dramatic secondary factors. For example severe gum bleeding is a common feature in acute leukemia and it can be the presenting feature of the disease.
Leukemia
Leukemia is a malignant neoplastic disease of white blood cells-forming tissues, usually with increased number of leucocytes in the circulation included are developing blast cells and other tissues including lymph nodes are infiltrated.
Two main types of leukemia
- Chronic leukemia commonly occurs in adults over 40,
- Acute leukemia commonly seen in children and young adults
The oral features reflect the white blood cells disturbance, and also the effects of treatment with radiotherapy and chemotherapy:
- Oral ulceration, petechiae (minute red or purple bleeding spots on the surface of the skin) and ecchymoses (large area of bleeding spots),
- Gum enlargement and gum bleeding,
- Bacterial, viral and fungal infections can lead to exacerbation of existing conditions such as acute necrotizing ulcerative gingivitis (ANUG) or increased in susceptibility to these gum disease.
Treatment of periodontal disease in leukemia
Effort should be made to provide treatment during remissions and professionally administered control is worthwhile. Chlorhexidine rinse regardless of staining should be used with antibiotic cover for invasive treatment and frank infections.