Continued from Part 1
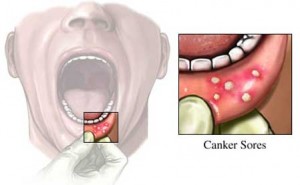
How is recurrent aphthous stomatitis diagnosed?
Diagnosis of recurrent aphthous stomatitis is based on the history and clinical features, as no specific tests are available. Biopsy is rarely indicted and is only usually needed where a different diagnosis is suspected. However to exclude the systemic disorders, it is useful to undertake investigations on blood (for example full blood picture) and serum (for example ferritin levels and vitamin B12 measurements).
How to differentiate between oral cancer ulcer and recurrent aphthous stomatitis?
If an ulcer in mouth has been present for more than 3 weeks, referral for appropriate specialist investigations, including biopsy is mandatory.
The presence or absence of pain is not particularly useful diagnostically although the character of the pain may be of value. Pain is often a late feature of oral carcinoma or mouth cancer and the fact that an ulcer may be painless never excludes it from being a potential oral cancer ulcer.

Oral cancer © toothiq.com
The oral cancer ulcer is described as a form with raised edges, with an indurated, inflamed, granular base and is fixed to surrounding tissues.
Oral cancer symptoms are most often seen as:
- A persistent painless ulcer that bleeds easily and does not heal
- A lump, thickening, rough spot, crust or small eroded area
- Color changes such as an area of white patch (leukoplakia), a red-white patch (erythroleukoplakia) or a red patch (eryhtroplakia),
- Difficulty in chewing, swallowing, speaking or moving the jaw or tongue
- Changes in the voice
- A change in the way your teeth fit together
- Pain, tenderness or numbness in the mouth or lips
- Signs of hardness or fixation of lesion
- Regional extension to draining lymph nodes
- As cancerous change of long-standing harmless (benign) tumors or rarely, cyst linings or a non-healing extraction socket.
Management of recurrent aphthous stomatitis
Recurrent aphthous stomatitis can be managed, though rarely cured, though the following methods:
1) Disorders where aphthous-like ulcers are also seen should be excluded:
- Behçet’s, Sweet’s and periodic fever, aphthous ulceration, pharyngitis and cervical adenitis (PFAPA) syndromes.
- Epstein Barr virus (EBV) infection
- Immunodeficiency syndromes
- Gastrointestinal diseases, especially celiac disease and Crohn’s disease
2) Predisposing factors should be corrected
- ensure trauma, hard or sharp foods are avoided and tooth brushing is atraumatic.
- if sodium lauryl sulphate (SLS) is implicated, this should be avoided.
- any iron or vitamin deficiency should be corrected
- if there is an obvious relationship to certain foods, these should be excluded from diet
- causal drugs should be excluded
3) Relief of pain and reduction of ulcer duration
Fortunately, the natural history of recurrent aphthous stomatitis  is one of eventual remission in most cases, therefore no treatment is probably the best option for an occasional ulcer. However remission may take several years and thus, oral ulcer treatment is indicated if the individual has significant discomfort.
Topical corticosteroids can often control recurrent aphthous stomatitis . The major concern of adrenal suppression with long term and/or repeated application has rarely been addressed, although the preparations noted below appear not to cause this problem:
- Topical hydrocortisone hemisuccinate pellets
- Topical triamcinolone acetonide in carboxymethyl cellulose paste
- Stronger topical corticosteroids for example betamethasone sodium phosphate
Topical tetracycline (doxycycline dissolved in water) as a mouth rinse may provide relief and reduce ulcer duration, but should be avoided in children under 12 years old who might ingest the tetracycline and develop tooth staining.
Good oral hygiene should be maintained, therefore chlorhexidine or triclosan mouthwashes may help.
There is a spectrum of topical anti-inflammatory agents such as benzydamine that may help in the management of discomfort in recurrent aphthous stomatitis.
If recurrent aphthous stomatitis fails to respond to these measures, systemic immunomodulators may be required, under specialist supervision. These include:
- Corticosteroids systemically (for example prednisolone)
- Levasomide
- Colchicine
- Thalidomide
Treatment regimens for recurrent aphthous stomatitis
Ulcer treatment |
Preparations available |
Particularly suitable for |
| Covering agents | Orabase
|
Reducing pain |
| Topical analgesics / anesthetics / anti-inflammatory agents | Benzydamine hydrochloride mouthwash or spray
Amlexanox
|
Reducing pain |
| Topical antiseptics | Doxycycline
Chlorhexidine gluconate
|
Hasten healing |
| Topical mild potency steroids | Hydrocortisone hemisuccinate
triamcinolone acetonide in carboxymethyl cellulose paste
|
Frequently recurring or severe ulcers |
| Topical moderate potency steroids | Beclomethasone dipropionate
Fluocinonide, clobetasol or betamethasone sodium phosphate
|
Inaccessible sites (for example soft palate) |
| Systemic agents | Oral prednisolone
Colchicines Pentoxifylline Azathioprine Thalidomide
|
Sever recurrent aphthous stomatitis or aphthous-like ulceration |
What is Behçet’s disease (syndrome)?
Behçet’s disease (syndrome) is characterized by recurrent aphthous stomatitis (RAS ) and at least two of the following: genital ulcers, eye lesions, skin lesions or rapid acute inflammation of skin in response to minor trauma. Lesions involving other body systems may also be seen. It is a rare disorder in Western countries and is seen mainly in countries from the eastern Mediterranean area to the Far East, corresponding to the route of the ancient silk traders.