Continued from Part 1
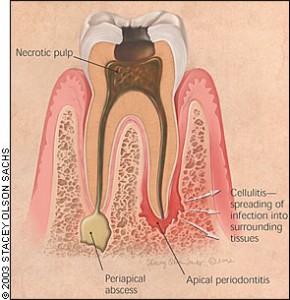
Acute periapical periodontitis
Pain associated with acute perapical periodontitis:
-
Is spontaneous in onset
-
Is moderate to severe in intensity
-
Persists for long periods of time (hours)
-
Is worsen by biting on tooth and in more advanced cases, even by closing the mouth and bringing the affected tooth gently into contact with the opposing teeth. In these cases, the tooth feels ‘high’ (extruded) and is sensitive to touch
-
Has often been preceded by pulpal pain
-
Is usually better tolerated than the sudden and excruciating pain of pulpitis
-
Is usually precisely localize and the individual is able to indicate the affected tooth. During examination the affected tooth is located readily by means of tooth percussion
-
Is usually associated with a non-vital tooth
-
Is usually associated with tenderness to palpation in the gum area near the root of the tooth
-
May be associated with swelling of the face. Caused by edema and cellulitis or sometimes connected with fever and body discomfort. Usually when the face swells, pain diminishes in intensity due to rupture of the pus through the periosteum of the bone around the affected tooth and the consequent decrease in pressure of tooth apex.
Lateral periodontal abscess
-
The pain is similar to that of acute periapical periodontitis, though often less severe and is well localized and with swelling and redness of the gums
-
However, the swelling is usually located more towards the gums than in the case of an acute periapical lesion which is around the root tip
-
The affected tooth is sensitive to percussion and is often loose and slightly extruded and there is a deep gum pocket. Probing the pocket may cause oozing of pus and subsequent relief from pain
-
The tooth pulp is usually vital
Food impaction
The cause of food impaction is usually a faulty contact between the teeth because of decay or poor restorations. Examination shows a faulty contact between the two teeth and often food trapped between these teeth, and the gum flap between the teeth involved is tender to touch and bleeds easily.
Food impaction between teeth can cause:
-
Localized pain that develops between or in two adjacent teeth after meals, especially when food is fibrous
-
Pain associated with a feeling of pressure and discomfort, which may gradually disappear until being evoked again at the next meal, or may be relieved immediately be removing the impacted food
-
The adjacent teeth to be sensitive to percussion
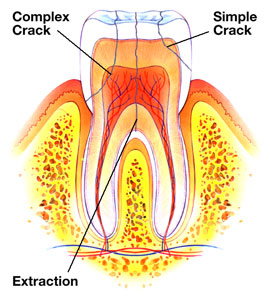
Cracked tooth
Examination may fail to draw out the cause of pain. Cracks may be revealed by biting on rubber or a Tooth Slooth, by fibre-optic or blue light illumination or by staining with, for example disclosing solution. Teeth can crack under trauma and can give rise to pain which is:
-
Severe
-
Worse on biting
-
Often precipitated by hot or cold
Pericoronitis
Acute infections around the crowns of teeth are common and are related to incompletely erupted teeth partially covered by flaps of gum tissue (operculum), particularly lower third molars or wisdom teeth.
-
Pain is spontaneous and is often worsen by closing the mouth.
-
In more severe cases, pain may be aggravated by swallowing and there may be trismus (limited mouth opening) and occasionally fever, swollen lymph nodes and body discomfort.
-
Examination shows an operculum that is acutely inflamed, red and swollen. Frequently, an opposing upper tooth indents or ulcerates the swollen operculum.
Acute necrotizing gingivitis
Examination shows necrosis and ulceration of the gums in between teeth in different degrees of marginal gum destruction. Similar features but with more intense pain may be seen in necrotizing periodontitis in HIV/AIDS.
Acute necrotizing gingivitis may cause:
-
Soreness and pain. In the early stages some individuals may complain of a feeling of tightness around the teeth. Pain is fairly well localized to the affected areas
-
Profuse gum bleeding
-
Bad breath, usually
-
Metallic taste, sometimes
-
Fever and body discomfort, sometimes
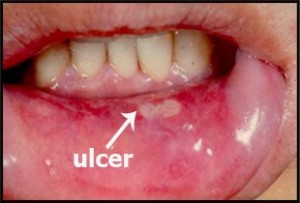
Mucosal pain
Pain from oral mucosal lesions can either be localized or diffuse, localized pain is usually associated with an erosion or ulcer. Diffuse pain may be associated with a widespread infection, mucosal atrophy or erosion, a systemic underlying deficiency disease or other factors, and is usually described as ‘soreness’ or sometimes ‘burning’. Mucosal pain may be aggravated mechanically by touch or by sour, spicy, salty or hot foods.
Other local causes of orofacial pain
Jaws
Pain from the jaws can be caused by acute infection, cancers, Paget’s diseae and direct trauma. Lesions such as cysts, retained roots and impacted teeth are usually painless unless associated with infection orfracture of the jaw. Odontogenic and other harmless tumors of the bone do not normally produce pain, but cancerous tumors usually produce deep, boring pain, sometimes associated with paraesthesia (partial numbness), hypoesthesia (decreased sensitivity) or anesthesia (complete numbness). Radiation therapy or bisphosphonate may result in severe jaw pain due to infection associated with osteonecrosis.
To be continued in Part 3